Basilar Invagination
Basilar Invagination
Last update: 31/05/2019, Dr. Miguel B. Royo Salvador, Medical Board number 10389. Neurosurgeon y Neurologist.
Definition
Basilar Invagination, or Basilar Impression, is the most frequent cervico-occipital junction malformation, therefore more often associated to neurological disorders of the cervicobulbar region. It consists in the invagination of the foramen magnum’s bone contour into the posterior cranial fossa, reducing its capacity and giving the skull base a cupular shape, opposite to the normal one (Convexobasia).
The foramen magnum is usually small, deformed and displaced upwards into the cranial cavity. The clivus is high. The atlas is under-developed, can be asymmetrical and usually attached to the occipital bone. The lamina can be partially formed. The odontoid and axis are projected forward and upward from their normal position and invade the spinal canal. The Basilar Invagination is often associated to Arnold-Chiari Syndrome type I and, less frequently, to Syringomyelia.
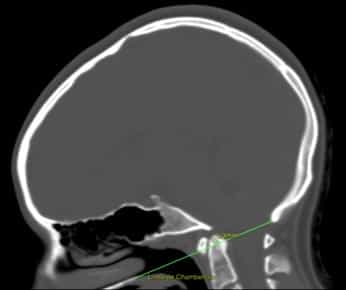
Figure.1 Basilar Invagination. Cranial CT scan with Chamberlain line, which joins the posterior edge of the foramen magnum (opisthion) with the posterior hard palate. It must touch the tip of the odontoid apophysis. In this case the line passes the tip by 5,3 mm.
Symptoms
Approximately half of the cases of Basilar Invagination are asymptomatic, while the other half can present side effects on the Nervous System. Clinically, it manifests with a short neck that tends to tilt forward and is hyperextended, stiff neck, limitation of cervical movements and constant cervico-occipital pain.
Neurological manifestations are typical of higher cervical cord compression: loss of strength and spasticity, gait instability, dysmetria and progressive sensory loss. It can be involved in a chronic intracranial hypertension.
Computer Tomography scan – Cranial CT scan
The Basilar Invagination is diagnosed and monitored through a computer tomography scan (cranial CT scan) or a cranio-cervical X-ray in profile view.
The diagnosis can also be made by means of a magnetic resonance of the skull, although for an optimal monitoring of the malformation, a CT scan or X-ray is recommended.
The diagnosis is established through Fischgold measurement, Fischgold and Metzger’s bimastoid line, Fischgold and Metzger’s digastric line, or the better known McGregor and Chamberlain lines (Fig.1).
Causes
– According to conventional theories:
- Idiopathic Basilar Invagination is considered to be a primary malformation and it is attributed to an early synostosis of spheno-occipital suture.
- Secondary Basilar Invagination can be determined by additional causes related to bone diseases such as: Rheumatoid arthritis, Hyperparathyroidism, Paget’s disease, alterations in osteogenesis, Rickets.
– According to the Filum System® health method:
The malformation observed in Idiopathic Basilar Invagination is produced by a congenital mechanism of growth asynchrony, in the embryonic stage, between the spinal cord and the central nervous system on one hand and the spine on the other. This generates an abnormal spinal cord traction that is transmitted through the filum terminale from the coccyx up to the cranium. The more intensely and early the traction is applied, the more relevant the bone manifestations of invagination.
Basilar Invagination shares cause – the traction generated by an overly tense Filum Terminale – with the Arnold-Chiari Syndrome type I, Idiopathic Syringomyelia and Idiopathic Scoliosis, and other related malformations of the occipital junction (all of them considered to be different manifestations of the Filum Disease).
Risk factors
The most influential risk factors for the development of Idiopathic Basilar Invagination are related to family history: it’s a congenital condition that can be inherited between family members. It shares the same genetic incidence of the Filum Disease, with a pathological mechanism that can be found in all human embryos. Its clinical manifestation depends on the intensity, context and form of expression of the mechanical conflict.
Complications
Complications of Basilar Invagination may depend on the degree of caudal traction or the consequent mechanical conflict in the foramen magnum. The latter affects the magnitude and intensity or degree of the conflict between the traction of the spinal cord and the brainstem.
- Deterioration of the Quality of Life: in the Basilar Invagination, stiff neck, limitation of cervical movements, constant cervico-occipital pain, loss of strength and spasticity, gait instability, dysmetria and progressive sensory loss, can become chronic, increase in intensity and deteriorate the patient’s state more and more, up to limiting their normal activity.
- Chronic pain: patients with Basilar Invagination may need to undergo treatment at a Pain Clinic, because the first choice anti-inflammatory or pain-killing drugs may not be enough to bear the symptoms of pain and headache crises characteristic of the disease
- Sudden death: can be produced due to injuries in the nuclei of cardiorespiratory functions in the brainstem, where the mechanical conflict takes place. Respiratory disorders while sleeping can constitute an aspect of the condition and can manifest as apnoea, respiratory failures or even in the sudden death of the patient. Hence, the importance of early diagnosis and treatment.
Treatment
The conventionally accepted treatment for Basilar Invagination is neurosurgical.
Currently, the craniectomy or suboccipital decompression is the standard treatment performed in most centres worldwide for this diagnosis. Usually it is indicated especially for severely symptomatic cases, as it causes more morbidity and mortality than the natural evolution of the condition itself.
Since 1993, however, with the publication of Dr Royo-Salvador’s doctoral thesis, which links the caudal traction of the entire nervous system due to the filum terminale to being the cause of the bone invagination – among other diseases – a new treatment has been designed. It is in this case etiological (cause-related) since the caudal cord traction force responsible for the pathological mechanism is eliminated by surgically sectioning the filum terminale.
Our technique for the sectioning of the Filum terminale (SFT) is minimally invasive and it is usually indicated as soon as possible in all cases, from mildly to severely symptomatic, as its risks are minimal, much lower than those of the condition itself, and it also stops the condition’s progression.
Minimally invasive Sectioning of the Filum Terminale according to the Filum System®:
Suboccipital Craniectomy
(Foramen magnum decompression)
Sectioning of the Filum terminale: Outcomes
More than 1500 patients with Filum Disease and Neuro-Cranio-Vertebral Syndrome have already undergone surgery according to the Filum System® method.
The purpose of the surgical procedure is to stop the evolution of the disease – in the case of Basilar Invagination especially the related neurological manifestations – to prevent the patients’ quality of life from getting worse.
References:
- Dr. Miguel B. Royo Salvador (1996), Siringomielia, escoliosis y malformación de Arnold-Chiari idiopáticas, etiología común (PDF). REV NEUROL (Barc); 24 (132): 937-959.
- Dr. Miguel B. Royo Salvador (1996), Platibasia, impresión basilar, retroceso odontoideo y kinking del tronco cerebral, etiología común con la siringomielia, escoliosis y malformación de Arnold-Chiari idiopáticas (PDF). REV NEUROL (Barc); 24 (134): 1241-1250
- Dr. Miguel B. Royo Salvador (1997), Nuevo tratamiento quirúrgico para la siringomielia, la escoliosis, la malformación de Arnold-Chiari, el kinking del tronco cerebral, el retroceso odontoideo, la impresión basilar y la platibasia idiopáticas (PDF). REV NEUROL; 25 (140): 523-530
- M. B. Royo-Salvador, J. Solé-Llenas, J. M. Doménech, and R. González-Adrio, (2005) “Results of the section of the filum terminale in 20 patients with syringomyelia, scoliosis and Chiari malformation“.(PDF). Acta Neurochir (Wien) 147: 515–523.
- M. B. Royo-Salvador (2014), “Filum System® Bibliography” (PDF).
- M. B. Royo-Salvador (2014), “Filum System® Guía Breve”.
Filum Disease
Dr. Royo-Salvador, with his research and doctoral thesis (1992), proved the theory that considers several diseases of unknown cause (Arnold-Chiari Syndrome Type I, idiopathic Syringomyelia, idiopathic Scoliosis, platybasia, basilar invagination, odontoid retroflexion, brain stem kinking, and others) as part of a new disease concept (the Filum Disease) and that they share a common cause (spinal cord and entire nervous system traction). When the cause of the mechanical conflict is not congenital, we talk about Neuro-Cranio-Vertebral Syndrome.
The traction force of the entire nervous system in the Filum Disease occurs in all human embryos, hence they all suffer its consequences to a greater or lesser extent, and the consequences manifest in many different ways and intensities.
Other diseases, such as herniated discs, some cerebral vascular insufficiency syndromes, facet joint and Baastrup syndromes, fibromyalgia, chronic fatigue, nocturnal enuresis, urinary incontinence and pronounced paraparesis, are related, due to their cause, to the Filum Disease.
A health method, the Filum System®, has been designed to specify the diagnosis, provide guidance for the treatment and follow-up of the Filum Disease.