COVID-19, the Filum Disease and the “brain fog”
Published by ICSEB at 29 December, 2020
In the current circumstances marked by the COVID-19 pandemic, many doubts may arise. Patients and family members are wondering, for example, whether people with Filum Disease can be considered a risk group for COVID-19.
At the Institut Chiari & Siringomielia & Escoliosis de Barcelona we would like to provide the most relevant and pertinent information that we have, to try and answer – and possibly solve – these doubts.
COVID-19 is a new condition with a very variable behaviour, making it difficult to identify the factors or circumstances responsible for its mortality or harmlessness.
Researchers and medical professionals are studying in COVID-19 all that is related to both the SARS CoV2 virus and the human host, that make this union so lethal for some patients.
One of the first scientific articles on the severity of COVID-19 is by Zsuzsanna Varga (Zurich, Switzerland) in The Lancet1 April 17 2020, which states the existence of an inflammation of the innermost layer of cells of the blood vessels – the endothelium – of various vital organs, such as the heart, brain and kidneys. There are currently 1680 articles COVID-19 endothelitis in general and 822 articles on COVID-19 brain endothelitis.
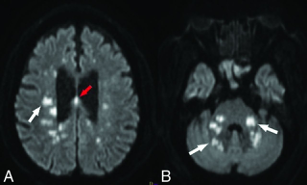
FIG 1. Diffuse ischemic lesions of the deep white matter. MRI visible diffusion (based on live detection of water molecule movement) in a patient with COVID-19, shows numerous focal ischemic lesions in the hemispheric deep white matter (A, white arrow), the corpus callosum (A, red arrow), basal ganglia, middle cerebellar peduncles and cerebellar hemispheres (B, white arrows) 2.
This inflammation, which appears in the brain endothelium of severe COVID-19 cases, (Fig.1), can cause in many patients a sensation of “brain fog”, a neurological alteration that is observed both in severe and mild patients. It is one of the long-term COVID-19 sequelae that more and pore people report having suffered or are still suffering, with significant consequences for their quality of life.
“Brain fog”, which includes difficulty with memory, concentration, speech and naming, confusion, dizziness, fatigue, may be aggravated in some patients with other brain lesions that favour or predispose to it, in the form of further inflammation or cerebrovascular accidents.
Our medical and research team described a new condition, the Filum Disease, in which a diffuse alteration in the cerebral blood circulation was observed, predominantly in the white matter areas (Figure 2) 3.
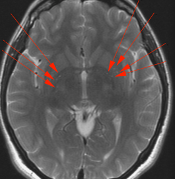
FIG 2. Diffuse ischemic lesions of the deep white matter. MRI of a patient with Filum Disease showing numerous focal ischemic lesions in the hemispheric deep white matter, the basal ganglia (red arrows), which disappeared after surgery.
We can assume that the predisposition to other brain injuries due to endothelitis can aggravate or increase sequelae in patients with COVID-19 and Filum Disease.
We know that this cerebral inflammatory predisposition of the Filum Disease can be solved with the surgical treatment proposed for it, therefore an early diagnosis with the application of the adequate treatment may be recommended.
There exist an additional problem, due to the fact that the Filum Disease, being a recently described condition, hardly diagnosed and apparently of wide global incidence, in general is unlikely to be taken into consideration in association with COVID-19.
References
- ZsuzsannaVarga , Andreas J Flammer , Peter Steiger , Martina Haberecker , Rea Andermatt , Annelies S Zinkernagel , Mandeep R Mehra , Reto A Schuepbach , Frank Ruschitzka , Holger Moch. Endothelial cell infection and endotheliitis in COVID-19. Case Reports. Lancet. 2020 May 2;395(10234):1417-1418.
- R Hanafi, P-A Roger, B Perin, G Kuchcinski, N Deleval, F Dallery, D Michel, L Hacein-Bey, J-P Pruvo, O Outteryck, J-M Constans. COVID-19 Neurologic Complication with CNS Vasculitis-Like Pattern. AJNR Am J Neuroradiol. 2020 Aug;41(8):1384-1387. doi: 10.3174/ajnr.A6651.
- The Filum disease and the Neuro-Cranio-vertebral syndrome: definition, clinical picture and imaging features. BMC Neurology 2020, May 15. 20:175. https://rdcu.be/b36Pi.