Tethered cord with spina bifida – meningocele or myelomeningocele – or Tethered Cord Syndrome
Definition
In normal conditions, the spinal cord is held within the spinal canal only by the denticulate ligaments and the filum terminale, a ligament that connects the conus medullaris to the first coccygeal vertebrae.
When the mobility of the spinal cord within the bony spinal canal is limited by the presence of an externally visible spina bifida that produces a tethering, the clinical picture is defined as Tethered cord syndrome with spina bifida or “Tethered Cord Syndrome”.
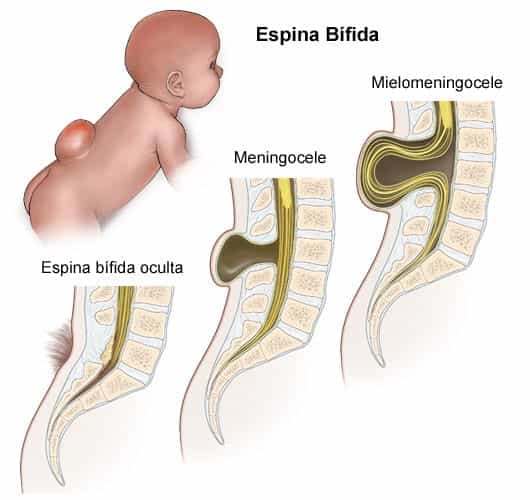
A spina bifida is defined as a neuro-spinal malformation that is characterized by the incomplete development of the spinal cord and manifests externally and/or internally, predominantly in the lumbar region. It is classified as a defect of the neural tube, which is the embryonic structure that ultimately becomes the baby’s brain and spinal cord and the tissues that enclose them.
In spina bifida with meningocele, the meninges – membranes that surround the spinal cord – protrude through the opening of the vertebrae and form a fluid-filled sac (Fig.1).
In “open” spina bifida with myelomeningocele, the spinal canal is open along several vertebrae in the lower or middle back (Fig.1). At birth, the membranes and spinal nerves protrude through this opening and form a sac on the baby’s back, usually exposing tissues and nerves and putting the baby’s life at risk.
In the tethered cord syndrome with spina bifida, the spinal cord is anchored by the malformation, producing mechanical injuries due to the traction applied to the whole nervous system, the cranium and vertebral column, associated with specific conditions like Arnold-Chiari syndrome type II, secondary scoliosis and syringomyelia.
Diagnosis
The diagnosis of tethered cord with spina bifida can be made prenatally. During pregnancy, prenatal testing is done to detect possible birth defects. For spina bifida detection, it includes:
- Blood tests:
- Maternal serum alpha-fetoprotein test.
- Test to confirm high levels of alpha-fetoprotein.
- Additional blood tests.
- Ultrasound: an ultrasound is performed when high levels of alpha-fetoprotein are detected.
- Amniocentesis: if alpha-fetoprotein levels are high but ultrasound is normal, an amniocentesis is usually recommended. When there is a neural tube defect, the amount of alpha-fetoprotein in the amniotic fluid is high.
Symptoms
Spina bifida symptoms vary depending on the severity of the case. The severity is determined by the size and location of the malformation, whether or not it is covered by the skin, whether spinal nerves protrude from it, and what nerve structure and nerves are involved.
In general, this malformation affects three of the main systems of the organism: the central nervous system, the locomotor system and the genitourinary system. It can cause various degrees of paralysis and loss of sensitivity in the lower extremities, as well as various complications in intestinal and urinary functions. Generally, all the nerves located below the malformation are affected. Therefore, the higher up the level of the malformation in the back, the greater the nerve damage and the loss of muscle function and sensitivity.
Causes
In general, the neural tube forms in the early stages of pregnancy and closes by day 28 after conception. In babies with spina bifida, part of the neural tube does not form or close properly, producing defects in the spinal cord and bones of the vertebral column.
Spina bifida is a congenital malformation, although with no pattern of inheritance. Although the elements and mechanisms that cause the neural tube’s incomplete closure are unknown, this malformation occurs during foetal development and is usually associated with the presence of low levels of folic acid during pregnancy.
Consequently, the cause of a tethered cord with spina bifida is attributed to a combination of genetic predisposition and environmental factors.
Risk factors
Some factors are associated with an increased risk of spina bifida with meningocele or myelomeningocele in the foetus:
- Family history of neural tube defects.
- Folate deficiency and of other metabolic agents.
- Diabetes.
- Obesity.
- Hyperthermia during pregnancy.
- Mother’s intake of some psychotropic medication during pregnancy, like anticonvulsants.
- Other environmental agents during pregnancy.
- Arnold-Chiari Syndrome type II.
- Hydrocephalus.
- Meningitis in newborns.
- Neurogenic bladder.
- Neurogenic bowel.
- Walking and mobility problems.
- Foot deformities.
- Other orthopaedic complications
- Possible learning disabilities have been observed in children with myelomeningocele and hydrocephalus.
- As children with spina bifida grow older, they can present additional problems, such as latex allergy, skin problems, gastrointestinal disorders and depression.
- Intrauterine surgery: the uterus is exposed and the baby’s spinal cord is opened and repaired. This surgery is performed before the 26th week of pregnancy, in prenatal surgery specialized centres with neonatal intensive care units and paediatric multidisciplinary teams. It allows to reduce premature births and the subsequent disease sequelae, be they infections or complications such as hydrocephalus, which would aggravate these sequelae.
- Surgical closure of the defect after birth: its objective is to prevent the secondary infection of the nervous tissue and any other possible trauma that the exposed spinal cord could suffer. Meningocele requires surgery to put the meninges back in place and close the vertebrae opening. Myelomeningocele implies a higher risk or damage for the involved nerves: it is closed by covering the exposed part with muscle and skin, in order to minimize the risk of infection of the exposed nerves. Sometimes a catheter or shunt is placed directly to control hydrocephalus.
- Treatment of complications: babies with myelomeningocele may need additional surgeries to treat complications. As they grow older, these patients may also need complementary therapies for bowel and bladder control, to walk or to move and for other autonomic functions, with the objective of improving their quality of life.
- Cahit Kural, Ilker Solmaz, Ozkan Tehli, Caglar Temiz, Murat Kutlay, Mehmet K. Daneyemez, Yusuf Izci. Evaluation and Management of Lumbosacral Myelomeningoceles in Children Eurasian J Med 2015; 47: 174-8
- Kenga Sivarajah, Sophie Relph, Radha Sabaratnam, Spyros Bakalis. Spina bifida in pregnancy: A review of the evidence for preconception, antenatal, intrapartum and postpartum care. Obstet Med. 2019 Mar; 12(1): 14–21. Published online 2018 May 17.
- Gutiérrez-Cabrera J., Pedroza-Ríos K. G., Cuéllar-Martínez S. Médula anclada en pacientes pediátricos y adolescentes. Revisión de 16 casos. Revista médica del Hospital General de México, S. S., Vol. 70, Núm. 2 Abr.-Jun. 2007 pp. 62-66.
- Lichtenstein B.W. Spinal dysraphism. Spina Bifida and myelodysplasia. Arch Neurol Psychiatry 44:792-809, 1940.
- Shokei Yamada. “Tethered cord Syndrome” American Association of Neurological Surgeons Publications Commitee 1996. ISBN 1-879284-37-5.
Complications
The first complication in a spina bifida with meningocele or myelomeningocele is the same tethered cord that it causes, with its early and progressive development.
Later on, other possible conditions are associated with this birth malformation, in a specific combination depending on each case:
Other complications may include:
Treatment
There can be different treatment approaches for tethered cord with spina bifida, depending on the moment it has been detected, its type and the associated conditions:
Bibliography
Understand the difference among the diagnoses of Tethered cord syndrome, Occult tethered cord syndrome y Filum Disease